|
|
|
This online tutorial series "Quality Improvement: Tool Time" reinforces practical
application of tools and competencies acquired during the live activity. Each Tool
is a combination of faculty commentary on essentials in clinical practice, links
to relevant scientific publications, and a printable handout that will serve as
a reminder. Please select the topic:
- Ensuring Quality of Care
- Optimizing Vancomycin for MRSA Infections
- Selecting Appropriate Therapy for ESBL- and KPC-Producers
- Dosing Strategies for MDR P. aeruginosa/A. baumannii Infections
- Adjusting Antimicrobial Regimens for Efficacy and Safety
|
|
Dosing Strategies for MDR P. aeruginosa/A. baumannii Infections
|
|
Rising Resistance Trends
|
|
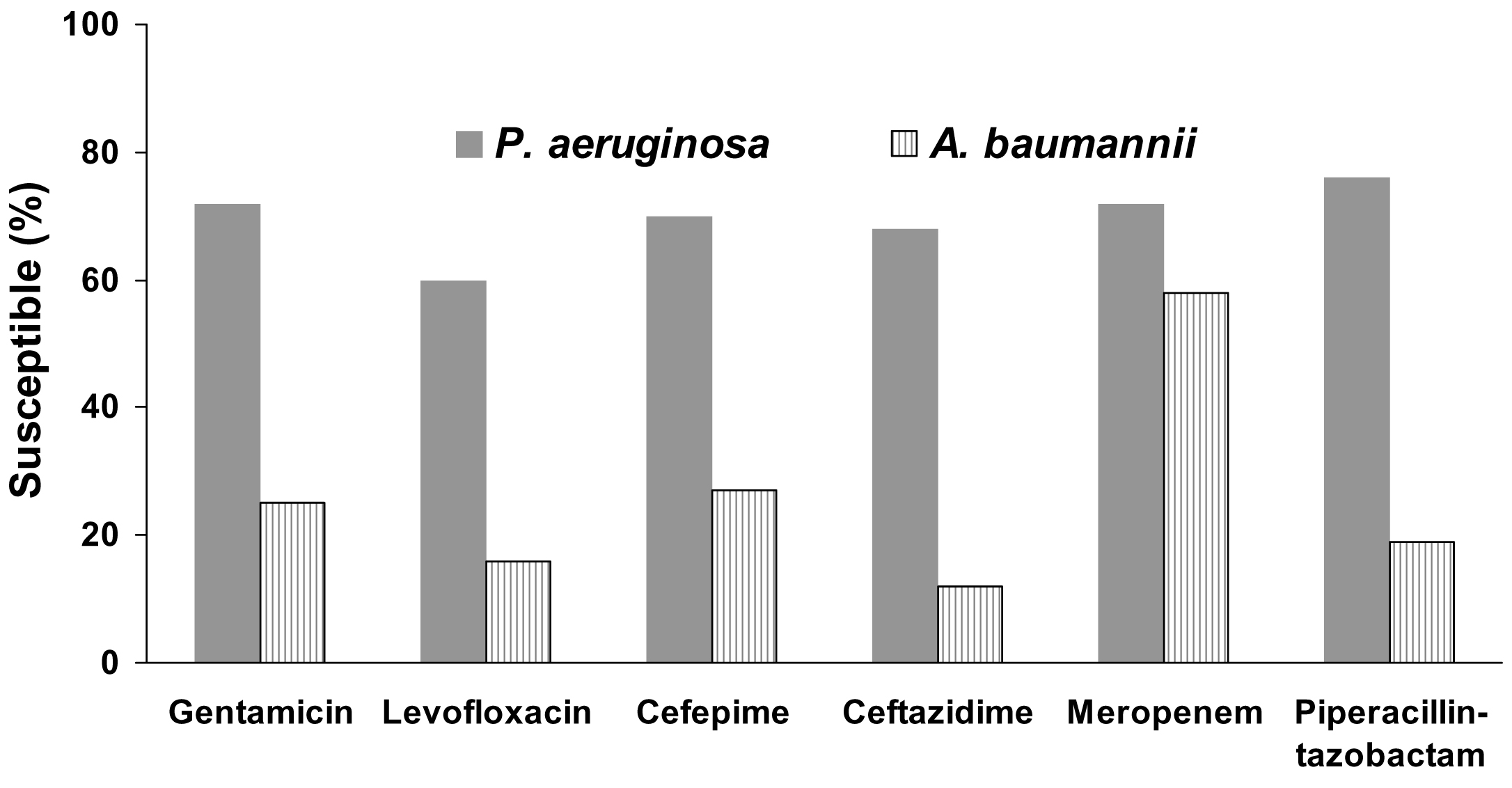
Pseudomonas aeruginosa and Acinetobacter baumannii present significant
challenges when managing hospital-acquired infections.
They are among the top 6 most frequently identified organisms causing
hospital-acquired bacterial pneumonia (HABP) and ventilator-associated
bacterial pneumonia (VABP).
[1]
Susceptibility of these pathogens to commonly used agents can vary
widely and no single agent is considered highly effective.
[1]
|

|
Dr. George Zhanel discusses current
resistance trends
|
|
|
Susceptibility Rates for HABP Isolates
SENTRY Antimicrobial Surveillance Program
2004–2008
|
|
|
Treatment Options and Dosing Strategies
|
|
As a consequence of lower than acceptable susceptibility rates, clinicians
typically utilize combination therapy when confronted with these pathogens.
Selecting the optimal combination should depend on local epidemiology and
based on the institutional antibiogram (or combination antibiogram,
if available).
[2]
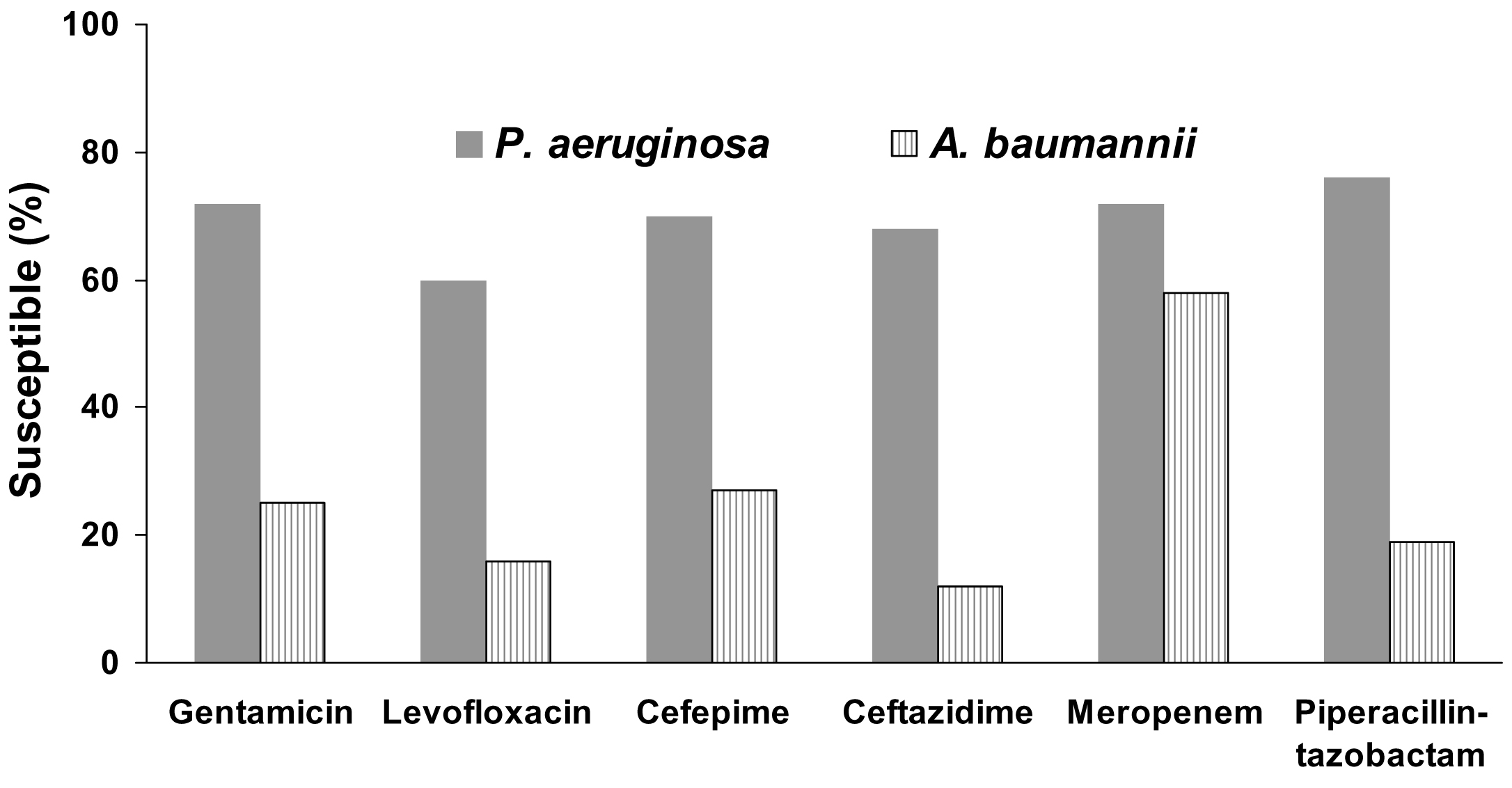
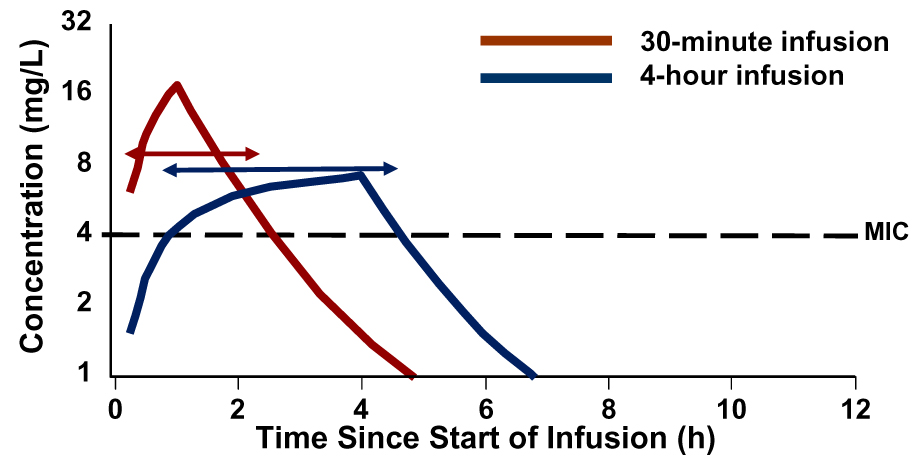
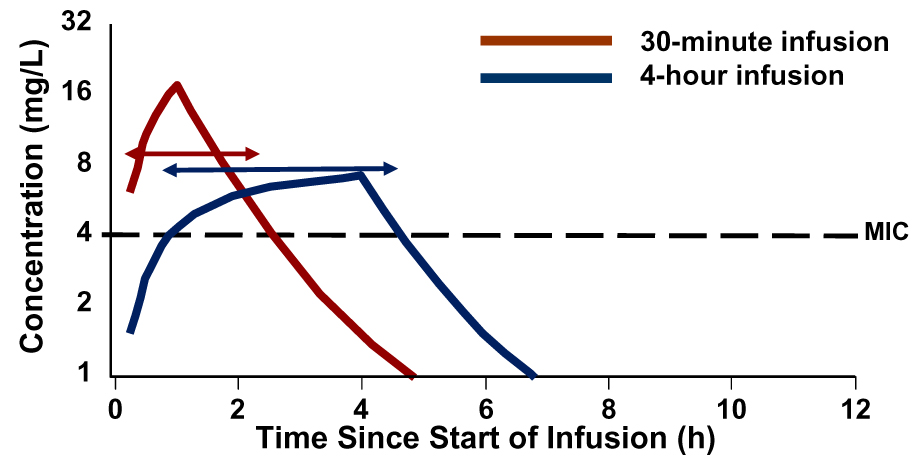
Optimized dosing strategies are also recommended to maximize the PK/PD
potential of antimicrobial agents. One well-studied tactic is the use
of prolonged infusions of β-lactams.
[3] This allows for a greater time
above the MIC (T>MIC) for the dosing interval without necessarily
increasing the dose administered.
|

|
Dr. Keith Rodvold discusses benefits
of prolonged infusion for β-lactams
|
|
|
PK of a β-lactam for Two Infusion Protocols
|
|
|
References
- Jones RN. Microbial etiologies of hospital-acquired bacterial pneumonia and
ventilator-associated bacterial pneumonia. Clin Infect Dis. 2010:51(Suppl 1):S81-S87.
Click here for abstract
- Christoff J, Tolentino J, Mawdsley E, Matushek S, Pitrak D, Weber
SG. Optimizing empirical antimicrobial therapy for infection due to Gram-negative
pathogens in the intensive care unit: utility of a combination antibiogram. Infect
Control Hosp Epidemiol. 2010;31:256-261.
Click here for abstract
- Crandon JL, Kuti JL, Jones RN, Nicolau DP. Comparison of 2002–2006 OPTAMA
programs for US hospitals: focus on Gram-negative resistance. Ann Pharmacother. 2009;43:220-227.
Click here for abstract
|
|
Suggested Reading
Rahal JJ. Antimicrobial resistance among and therapeutic options against Gram-negative
pathogens. Clin Infect Dis. 2009;49(Suppl 1):S4-S10.
Click here for complete article
This article provides an overview of resistance trends for common Gram-negative
pathogens causing nosocomial infections. A review of the mechanisms of resistance
to β-lactams is followed by recommended treatment strategies—combination therapy
followed by de-escalation and optimized dosing by extending the infusion period
for β-lactams.
Nicasio AM, Eagye KJ, Kuti EL, Nicolau DP, Kuti JL. Length of stay and hospital
costs associated with a pharmacodynamic-based clinical pathway for empiric antibiotic
choice for ventilator-associated pneumonia. Pharmacotherapy. 2010;30:453-462.
Click here for abstract
This retrospective analysis compared ICU costs before and after a clinical pathway
was implemented to optimize antibiotic regimen selection for ventilator-associated
pneumonia. The clinical pathway involved using a 3-drug regimen based on local MIC
distributions and a pharmacodynamically optimized dosing strategy using prolonged
infusions of β-lactams. This approach resulted in a shorter length of ICU stay, shorter
hospital length of stay, and lower hospital costs after VAP.
Sengstock DM, Thyagarajan R, Apalara J, Mira A, Chopra T, Kaye KS. Multidrug-resistant
Acinetobacter baumannii: an emerging pathogen among older adults in community hospitals
and nursing homes. Clin Infect Dis. 2010;50:1611-1616.
Click here for abstract
This study describes the epidemiology, resistance patterns, and outcomes of Acinetobacter
infections in older patients in community hospitals in suburban Detroit cities over a
6-year period (2003–2008). During this period, the prevalence of Acinetobacter infections
increased 25%. Resistance to imipenem and ampicillin/sulbactam increased from 1.8% (2003)
to 33.1% (2008). Pan-resistance (resistance to all 8 antibiotics tested) increased from 0% (2003)
to 13.6% (2008). A major concern was that many patients with resistant isolates were selectively
discharged to nursing homes and long-term care facilities, thereby introducing resistance in
these facilities.
|
|